Bridging Science and Surgery: Dr Nicholas Candy
.png)
Dr Nicholas Candy’s Journey as a Surgeon-Scientist
The NeuroSurgical Research Foundation (NRF) proudly supports emerging clinician-researchers dedicated to improving patient outcomes through innovation and collaboration. One such researcher is Dr Nicholas Candy, a neurosurgical accredited registrar currently based at the Royal Brisbane and Women’s Hospital.
Dr Candy whose work is funded through the Abbie Simpson Clinical Fellowship, has balanced the demands of neurosurgical training with a PhD focused on advancing outcomes for patients undergoing endoscopic pituitary surgery. We sat down with Dr Candy to discuss his research journey, inspirations, and the impact of NRF support on his work.

Dr Candy presenting at ANZPA meeting 2024.
What inspired you to pursue a PhD alongside your clinical training in neurosurgery?
Early on in my training I knew I wanted to be a surgeon-scientist. Complex skull-base and pituitary disorders sit at the intersection of delicate anatomy, demanding operations, and unanswered biological questions, precisely the kind of problems that benefit from careful science as much as skilled surgery. Pursuing a PhD allowed me to deepen my understanding of these diseases, build translational research skills, and keep patient outcomes, not just operative success, as a focus of training. I’ve been fortunate to learn from exceptional mentors who modelled how rigorous research can directly inform safer surgery and better recovery. Combining operating theatre experience with laboratory and data-driven inquiry felt like the most direct route to improve patient care.
Why did you choose to subspecialise in skull-base surgery and endocrine outcomes in pituitary surgery?
Pituitary adenomas (PitNETs) are among the most common primary brain tumours, and yet aspects that matter enormously to patients, long-term hormone control and durable remission, are comparatively under-reported. Historically, research focused first on access (endoscopic techniques) and then on reducing complications. The next leap is optimising outcomes: understanding which technical, anatomical, and team factors best predict endocrine success and how we can standardise them. Skull-base surgery also benefits from close multidisciplinary collaboration with endocrinology, ENT, radiology, pathology and oncology. That team science, and the chance to translate research into practical improvements at the point of care, is what drew me to this field.
Could you briefly summarise your PhD research for the general public, the key findings, and any practical implications?
My PhD set out to improve hormone outcomes for people undergoing endoscopic pituitary surgery. I began by defining real-world endocrine results in South Australia and how they evolve over time, then explored how subspecialisation, surgical experience, and collaborative care relate to those outcomes. I evaluated ways to make image-guided surgery even more precise, because millimetres matter at the skull base. To strengthen training, I developed and tested high-fidelity 3D-printed models that realistically reproduce endoscopic pituitary surgery, aiming to flatten the learning curve in a safe environment. Finally, I initiated work toward fluorescent-guided surgery by investigating fluorophores that might one day help distinguish tumour from normal gland in real time.
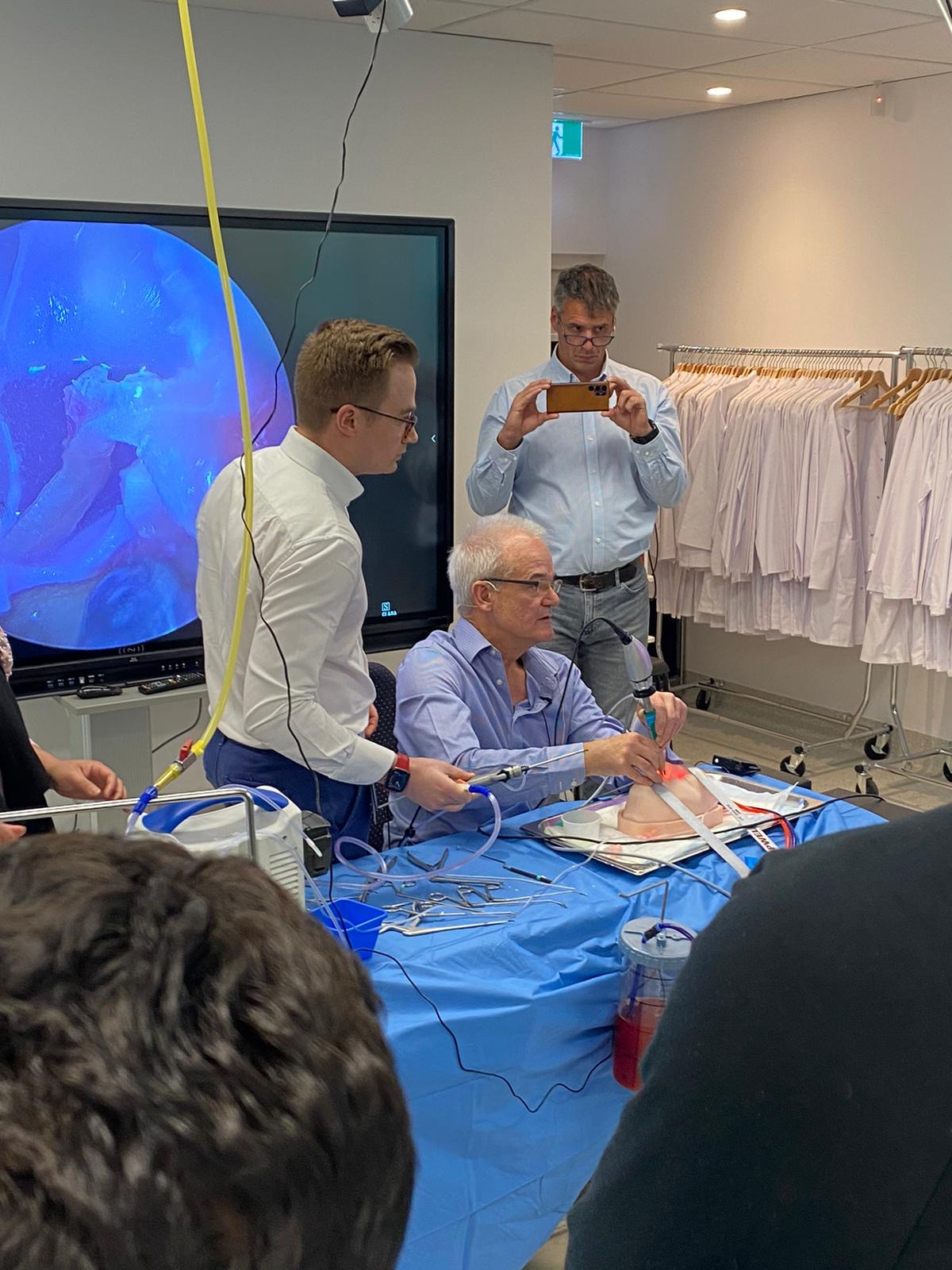
Demonstrating the 3D printed model at the 1st Endoscopic Pituitary Surgery Course in 2023
What advice would you give to young neurosurgeons or medical researchers aiming to combine clinical work with research?
I believe it’s crucial to begin your research with a question that genuinely interests you, as this will make the entire process enjoyable and engaging. Additionally, it’s highly beneficial to have a diverse group of mentors from both clinical and academic backgrounds.
How has the NRF supported your research?
The NRF’s support has been pivotal. As the Abbie Simpson Clinical Fellow, I received research funding and stipend support that made full-time PhD work possible during time away from neurosurgical training. That investment funded laboratory experiments, simulator development, and the analytical infrastructure behind our outcomes work. Equally important, the NRF community opened doors, linking clinicians, scientists and supporters, so that promising ideas could become practical studies faster.
How do you see your research evolving in the next few years, particularly regarding patient care or surgical innovation?
We’re moving into a more targeted, translational phase. In the laboratory, we are systematically profiling cell-surface (membrane) proteins in non-functioning pituitary tumours versus normal pituitary to shortlist a small number of specific targets. The goal is to enable monoclonal-antibody-based fluorescent guidance in endoscopic surgery, helping surgeons see tumour more clearly and preserve normal gland. This will ideally improve endocrine outcomes for patients by allowing higher rates of hormonal control and reduced rates of pituitary gland damage during surgery.
Any personal reflections or anecdotes you’d like to share about your PhD journey or your aspirations moving forward?
Looking ahead, I aim to return from overseas skull-base fellowships and work as a surgeon-scientist in a collaborative multi-disciplinary team.
You are based in Queensland at the moment. Are you planning to return to Adelaide?
Yeah that’s right, I am currently at the Royal Brisbane and Women’s Hospital completing my second last year of training. We are required to move interstate for at least one year of our training to ensure we get a well rounded exposure during training. I am going to be at FMC in 2026 for my final year of training.
I found the excerpt below in article from Sheldon College which mentions that you setup SA's first statewide skull base multidisciplinary meeting, is this group still running?
"In 2020, Nicholas established South Australia’s first-of-its-kind, statewide skull base multidisciplinary meeting, which occurs every fortnight involving skull base surgeons and associated specialties from all tertiary hospitals within South Australia."
That’s right too. I started off a statewide skull base meeting, growing it from 2020 into a full statewide meeting with neurosurgery, radiation oncology, radiology, endocrinology, otology and rhinology. I chaired it up until I left SA at the end of 2024, but the meeting still runs with Dr Chris Ovenden and Dr Peter Gorayski as co-chairs. I will help with its running next year in 2026 when I am back in SA, but will spend the first half of the year focusing on my fellowship exams for training.
Dr Nicholas Candy
MBBS MSurg (Neurosurgery) PhD
Neurosurgical Accredited Registrar
Royal Brisbane and Women’s Hospital, Brisbane, Australia